INVASIVE CERVIAL RESORPTION
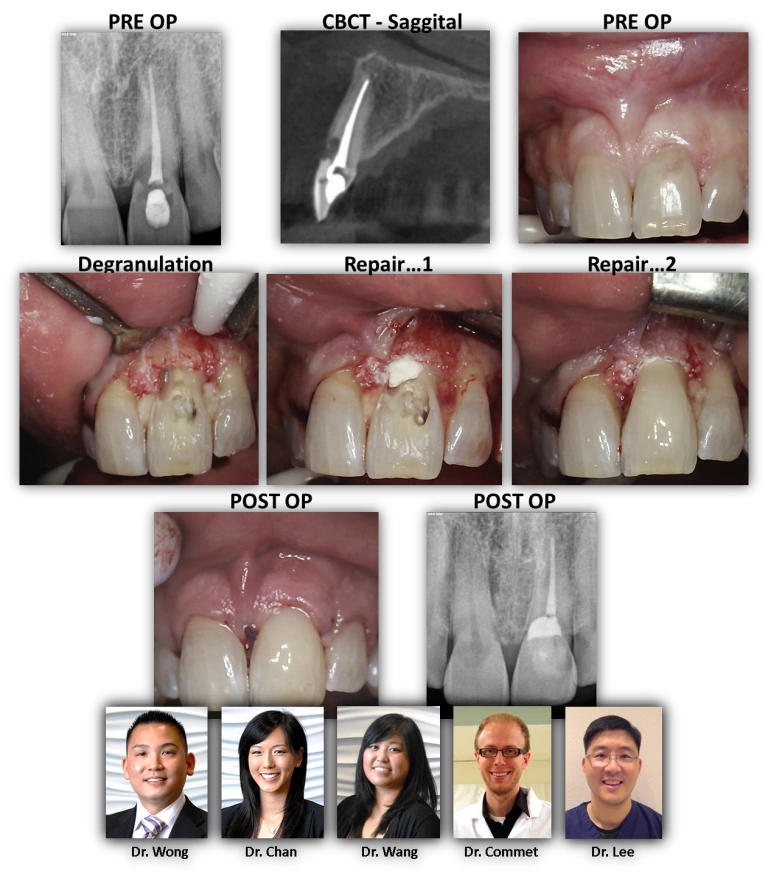
INVASIVE CERVICAL RESORPTION: Here is an interesting case. This patient ended up in our care after a root canal was done on tooth #9. He was informed at that time that it wasn’t guaranteed that the tooth could be saved and that a dental implant might be necessary or a surgery of some sort. As one can see on the pre-operative radiographs, sagittal slice of the CBCT and clinical photo, there is clear evidence of invasive cervical resorption on the buccal aspecdt extending below… the level of the crest. Additionally, the granulation tissue was not addressed via non-surgical access. Because the root canal had already been done, we took a surgical approach using a buccal full thickness mucoperiosteal flap and carefully remove the granulation tissue while not disturbing the cortical bone. We then filled the defect that was left with Brasseler Root Repair Material up to the level of the alveolar crest. We then placed core composite mixed the flowable composite (for esthetics) and shaped/smoothed prior to replacing the soft tissue flap with a couple of sling sutures. We then reaccessed the tooth and removed some of the root obturant to evaluate for root contaminant and any possibility of remaining resorption defect. The endodontic access was then restored with core composite. We feel that this case was managed well in terms of the pathology present while still maintaining the esthetic requirements that most patients have, particularly on a maxillary central incisor!